Public Health System Explained
Public Health System Explained: Primary to Tertiary Care
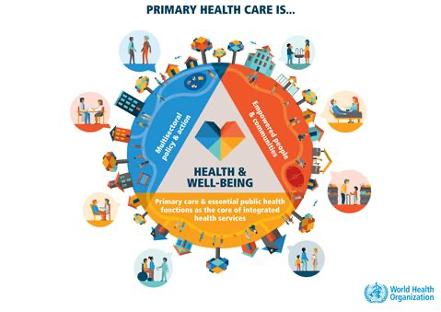
The World Health Organization emphasizes that well-organized healthcare systems built on strong primary care can address up to ninety percent of health needs while improving outcomes and reducing costs. When primary care is robust and accessible, it prevents many conditions from progressing to stages requiring expensive interventions at secondary or tertiary levels. This is not just theoretical - countries like Denmark, the Netherlands, and parts of Canada have demonstrated that investing in primary care infrastructure creates healthier populations at lower per capita costs than systems that rely heavily on hospital-based care.
But here is what makes this particularly relevant right now: India has undergone a dramatic transformation in healthcare delivery over the past decade. The country has established over 1.77 lakh Ayushman Arogya Mandirs, expanded free diagnostics and medicines, launched comprehensive insurance coverage through PM-JAY, and created digital health infrastructure that connects care levels like never before.
The Universal Logic of Tiered Healthcare Systems
Healthcare systems worldwide organize services into distinct levels not by accident, but through decades of evidence showing this structure delivers better outcomes more efficiently than unorganized approaches. The fundamental principle is matching patient needs with appropriate resources while ensuring accessibility and preventing both underuse of necessary services and overuse of expensive ones.
Why Healthcare Systems Organize Into Levels
The tiered approach reflects basic epidemiological reality: most health problems are common and can be managed with basic interventions, while a smaller proportion require specialized expertise and expensive technology. Research consistently shows that approximately eighty to ninety percent of healthcare encounters can be effectively handled at the primary care level. This includes acute conditions like respiratory infections and minor injuries, chronic disease management such as diabetes and hypertension, preventive services including vaccinations and health screenings, and coordination of care when higher-level services are needed.
This distribution means that healthcare systems achieve maximum population health benefit by ensuring robust primary care infrastructure is widely accessible, while concentrating specialized resources at secondary and tertiary levels where they can serve larger geographic areas efficiently. Countries that have built strong primary care foundations consistently outperform those that have invested primarily in hospital-based care, achieving better population health outcomes at lower per capita costs.
Global Models and Variations
Different countries organize their healthcare systems through various funding and delivery mechanisms, but most successful systems incorporate some version of the primary-secondary-tertiary structure. The United Kingdom's National Health Service represents the Beveridge model, where government directly provides and funds healthcare through taxation, with strong primary care gatekeeping that requires referrals for specialist services. Germany and France employ the Bismarck model, using social insurance funded through employer and employee contributions while maintaining clear care level distinctions.
Nordic countries like Denmark and Norway have achieved exceptional results by investing heavily in primary care infrastructure and ensuring that generalist physicians handle the vast majority of healthcare needs. These systems consistently rank among the world's best while spending less per capita than countries with weaker primary care systems. Canada's single-payer model combines public insurance with primary care emphasis, though with some challenges in specialist access that highlight the importance of adequate capacity at all levels.
The Economics of Appropriate Care Delivery
The economic logic of tiered healthcare is compelling. Primary care interventions typically cost a fraction of secondary care services, which in turn cost less than tertiary care. But the economics go beyond simple cost comparisons - they involve preventing expensive complications through early intervention, reducing emergency department utilization through accessible primary care, and ensuring that expensive specialized resources focus on cases that truly require them.
World Health Organization analysis demonstrates that every dollar invested in primary care prevention can save between three and seven dollars in downstream treatment costs. This is particularly relevant for chronic diseases like diabetes, hypertension, and heart disease, where primary care management can prevent complications that would require expensive hospitalizations and procedures.
Evidence for Primary Care Effectiveness
Research from multiple countries confirms that healthcare systems with strong primary care foundations achieve better outcomes across multiple metrics. These systems show lower rates of preventable hospitalizations, better management of chronic diseases, higher patient satisfaction, and more equitable access to care across different population groups.
The evidence also shows that primary care effectiveness depends on several key factors: geographic accessibility with services located close to where people live and work, financial accessibility with minimal barriers to seeking care, comprehensive services that address the full spectrum of common health needs, and strong referral relationships with secondary and tertiary levels that ensure seamless transitions when needed.
Primary Care - The Foundation and First Contact
What Primary Care Covers Worldwide
Primary care scope is remarkably broad, requiring providers to be skilled generalists with deep knowledge across multiple medical disciplines. The World Health Organization defines primary care as providing person-centered care over time for all but very uncommon or unusual conditions, with functions including health promotion and illness prevention, care of common episodic conditions, ongoing care for chronic conditions, and coordination of care when specialist services are needed.
This breadth means primary care providers manage acute illnesses like respiratory infections, gastrointestinal problems, skin conditions, and minor injuries. They provide ongoing care for chronic conditions including diabetes, hypertension, depression, anxiety, and arthritis. They deliver preventive services such as vaccinations, health screenings, lifestyle counseling, and risk factor modification. They also serve as the medical home that coordinates care when patients need services from other parts of the healthcare system.
Primary care's longitudinal relationship with patients and families creates opportunities for personalized care that considers individual risk factors, family history, social circumstances, and patient preferences. This relationship enables primary care providers to detect health problems early, provide anticipatory guidance, and support patients through health transitions.
India's Health and Wellness Centres and Ayushman Arogya Mandirs
India has transformed its primary care infrastructure through the creation of Health and Wellness Centres, now rebranded as Ayushman Arogya Mandirs under the Ayushman Bharat program. According to official parliamentary responses, more than 1.77 lakh such centers have been operationalized nationwide, representing one of the world's largest primary healthcare expansion initiatives.
These centers upgrade existing Sub Health Centres and Primary Health Centres to provide comprehensive primary healthcare services. The transformation involves expanding infrastructure, enhancing equipment and supplies, training additional workforce including Community Health Officers, and implementing expanded service packages that go far beyond the traditional focus on maternal and child health and communicable disease control.
The Ayushman Arogya Mandir concept emphasizes accessibility, with policy guidelines aiming for centers to be within reasonable travel time for all populations. In rural areas, this typically means Sub Health Centres serve populations of approximately 5,000 people, while Primary Health Centres serve around 30,000 people. Urban areas have different population norms but follow the same principle of geographic accessibility.
Comprehensive Primary Healthcare Package
The comprehensive primary healthcare package delivered through Health and Wellness Centres includes twelve service domains that collectively address most healthcare needs throughout the life course. These services span reproductive, maternal, newborn, child, and adolescent health services including antenatal care, safe delivery services, immunizations, and adolescent health counseling.
Communicable disease management covers tuberculosis, malaria, dengue, chikungunya, and other locally prevalent infections through prevention, early detection, treatment, and contact tracing. Non-communicable disease services focus on hypertension, diabetes, and common cancers through screening, treatment, and follow-up care.
Mental health services include counseling, treatment for common mental health conditions, and referral for specialized care when needed. Basic emergency medical care provides first aid, stabilization, and referral for serious emergencies. The package also includes oral health, eye care, ear care, and basic skin condition management.
Essential medicines and diagnostics support these services, with standardized lists that ensure common conditions can be diagnosed and treated at the primary level without requiring patients to seek private sector services or travel to distant facilities.
Screening, Prevention, and Community Health
Population-based screening programs represent one of primary care's most important but often invisible functions. India's national program for prevention and control of non-communicable diseases establishes screening protocols for adults beginning at age thirty, including blood pressure measurement for hypertension detection, blood glucose testing for diabetes screening, and clinical examinations for oral, breast, and cervical cancers.
These screening programs follow evidence-based guidelines that balance benefits and harms, focusing on conditions where early detection leads to better outcomes and where effective treatments are available. The programs also emphasize risk factor counseling, helping people modify tobacco use, alcohol consumption, diet, and physical activity patterns that contribute to chronic disease development.
Community health approaches extend primary care beyond facility walls through Accredited Social Health Activists and other community health workers who provide health education, support treatment adherence, and connect communities with facility-based services. This community connection helps primary care address social determinants of health and reach populations that might otherwise face barriers to accessing care.
Population Health Management and Accessibility
Effective primary care takes a population perspective, working to improve health outcomes for entire communities rather than just individuals who seek care. This involves identifying high-risk populations, conducting outreach to ensure preventive services reach those who need them most, and addressing community-wide health challenges through coordinated interventions.
Accessibility remains fundamental to primary care effectiveness. Geographic accessibility means locating services close to where people live and work, with transportation support when needed. Financial accessibility involves reducing cost barriers through free or subsidized services. Cultural accessibility requires services that are respectful of local customs and available in local languages. Temporal accessibility means providing services at times that accommodate work schedules and family responsibilities.
India's approach to accessibility emphasizes equity, with additional resources directed toward tribal areas, hilly regions, and other underserved populations. The goal is ensuring that zip code or socioeconomic status does not determine access to essential healthcare services.
Secondary Care - Specialized Services and Regional Hubs
Specialist Services and Referral Medicine
Secondary care encompasses the work of medical specialists who have additional training beyond general medicine or family practice. These specialists focus on specific organ systems, types of conditions, or patient populations. Common secondary care specialties include internal medicine subspecialties like cardiology, pulmonology, and gastroenterology; surgical specialties like general surgery, orthopedics, and urology; and other fields like psychiatry, dermatology, and ophthalmology.
The referral system is central to how secondary care functions effectively. In well-organized healthcare systems, patients access secondary care through referrals from primary care providers who have determined that specialist evaluation or treatment is needed. This referral process serves multiple functions: it ensures appropriate utilization of specialist services, maintains communication between care levels, and helps specialists understand the clinical context and previous interventions.
Effective referral systems require clear criteria for when referrals are appropriate, standardized communication processes between referring and receiving providers, and feedback loops that inform primary care providers about specialist recommendations and follow-up needs. When referral systems work well, they ensure patients get specialist care when needed while preventing overuse of expensive specialist services for conditions that could be managed in primary care.
India's Community Health Centres as Bridges
Community Health Centres represent the first hospital-level care in India's public healthcare system, typically serving populations of approximately 120,000 people in rural areas. These facilities are designed to provide secondary care services including specialist consultations, inpatient beds, surgical facilities, and emergency services.
Indian Public Health Standards for Community Health Centres specify service requirements including four specialist physicians in surgery, medicine, obstetrics and gynecology, and pediatrics, along with supporting staff including nurses, technicians, and administrative personnel. Infrastructure standards cover inpatient beds, operating theaters, labor rooms, emergency departments, and diagnostic facilities including laboratory and imaging services.
Community Health Centres serve as referral destinations for multiple Primary Health Centres in their catchment areas, handling cases that exceed primary care capacity while referring more complex cases to district hospitals or tertiary facilities. This hub and spoke model helps ensure that specialized services are available within reasonable geographic reach while concentrating resources efficiently.
The bridge function of Community Health Centres is particularly important in rural areas where geographic distances to tertiary care facilities may be substantial. These facilities provide emergency stabilization, common surgical procedures, complicated deliveries, and specialist consultations that reduce the need for patients to travel to distant urban centers for many secondary care needs.
District Hospitals and Regional Integration
District hospitals represent the major secondary care facilities in India's public healthcare system, typically serving entire districts with populations ranging from several hundred thousand to over a million people. These hospitals provide comprehensive secondary care services including multiple medical and surgical specialties, advanced diagnostic capabilities, intensive care services, and emergency departments.
Indian Public Health Standards for district hospitals specify detailed requirements for clinical departments, support services, infrastructure, and equipment. These standards ensure that district hospitals can handle the full range of secondary care needs including complex medical conditions, surgical procedures, high-risk pregnancies, pediatric emergencies, and trauma cases.
District hospitals also serve important functions beyond direct patient care, including training and supervision of healthcare workers from lower-level facilities, serving as referral sources for specialty consultations at Primary Health Centres and Community Health Centres, and coordinating emergency medical services and patient transport within their districts.
The regional integration function involves connecting district hospitals with both the primary care facilities they support and the tertiary care institutions they refer to for the most complex cases. This integration requires well-functioning communication systems, standardized protocols for referrals and transfers, and coordination of resources across facilities.
Emergency Services and Inter-facility Coordination
Emergency medical services represent the connective tissue that holds healthcare levels together, particularly for urgent and critical care needs. India's emergency medical services have evolved from simple transportation to comprehensive pre-hospital medical care, with trained personnel who can provide life-saving interventions during transport and coordinate with receiving hospitals.
National Health Mission guidelines for emergency medical services emphasize rapid response times, appropriate clinical protocols for common emergency conditions, and seamless handovers to receiving facilities. The system includes both emergency response to incidents and inter-facility transfers when patients need services at higher levels of care.
Emergency services coordination involves several key components: centralized dispatch systems that can mobilize appropriate resources quickly, communication systems that connect ambulance crews with medical direction and receiving hospitals, standardized protocols for common emergency conditions, and quality improvement processes that track response times and patient outcomes.
The effectiveness of emergency services depends heavily on coordination between care levels, including primary care facilities that can provide initial stabilization, secondary care hospitals that can handle most emergency conditions, and tertiary care centers that provide the most advanced emergency interventions.
Tertiary Care - Advanced Treatment and Academic Medicine
Complex Medical and Surgical Interventions
Tertiary care encompasses procedures and treatments that require significant specialized expertise, expensive equipment, and comprehensive support teams. These interventions include complex surgeries like organ transplants, cardiac surgery, neurosurgery, and cancer operations that require specialized surgical teams, advanced anesthesia services, and intensive post-operative care.
Medical interventions at the tertiary level include advanced cancer treatments like chemotherapy, radiation therapy, and immunotherapy; complex cardiac procedures like angioplasty and bypass surgery; neurological interventions for conditions like stroke, seizures, and movement disorders; and intensive care for critically ill patients requiring life support and specialized monitoring.
The complexity of tertiary care means that individual cases often require multidisciplinary teams including multiple specialists, specialized nurses, pharmacists, therapists, and other healthcare professionals working together. Treatment plans may involve coordination between different departments and services within the same institution, and care episodes may extend over weeks or months.
Advanced diagnostic capabilities support tertiary care interventions, including sophisticated imaging like magnetic resonance imaging, computed tomography, and nuclear medicine studies; complex laboratory tests including genetic testing, specialized pathology, and advanced microbiological studies; and interventional procedures that combine diagnostic and therapeutic functions.
Medical College Hospitals and Teaching Integration
Medical college hospitals serve the dual function of providing tertiary care services while training the next generation of healthcare professionals. These institutions integrate clinical care, medical education, and research in ways that advance medical knowledge while serving patients with complex conditions.
The teaching mission of medical college hospitals means they typically handle a disproportionate share of complex and rare conditions, as these cases provide valuable learning opportunities for medical students, residents, and fellows. This teaching function also means these hospitals often have access to the latest medical knowledge and techniques through their academic affiliations.
Research activities in medical college hospitals contribute to advancing medical science while potentially providing patients access to cutting-edge treatments through clinical trials and innovative procedures. The research mission also means these institutions often have expertise in rare conditions and experimental treatments that may not be available elsewhere.
The academic mission requires medical college hospitals to maintain high standards of clinical care while documenting and analyzing outcomes to contribute to medical knowledge. This dual mission can create tensions between efficiency and education, but it also drives continuous improvement and innovation in patient care.
Resource Intensity and Geographic Concentration
Tertiary care requires substantial investments in specialized personnel, advanced equipment, and complex infrastructure that make these services expensive to provide and maintain. The high cost per case means that tertiary care facilities must serve large populations to achieve financial sustainability, which typically results in geographic concentration in major urban centers.
This geographic concentration creates accessibility challenges, particularly for rural populations who may need to travel substantial distances to access tertiary care services. Healthcare systems address this challenge through various mechanisms including patient transport services, telemedicine consultations that can guide care at lower levels, and mobile specialty clinics that bring some tertiary services to underserved areas.
The resource intensity of tertiary care also means that these facilities require careful coordination with lower levels of care to ensure appropriate utilization. When primary and secondary care systems function well, they can handle many conditions that might otherwise present to tertiary facilities, allowing tertiary resources to focus on cases that truly require advanced interventions.
Geographic concentration also enables tertiary facilities to maintain the case volumes necessary for clinical teams to maintain expertise in complex procedures. High-volume centers typically achieve better outcomes for complex procedures than low-volume centers, supporting the rationale for concentrating advanced services in regional centers.
Integration, Referrals, and Digital Health Connectivity
Referral Systems and Patient Flow Management
Effective referral systems function as the circulation system of healthcare delivery, ensuring patients flow smoothly between care levels based on medical need rather than arbitrary factors. Well-designed referral systems include clear criteria for when patients should be referred to higher levels of care, standardized communication processes that ensure receiving providers have necessary clinical information, and defined pathways for different types of conditions.
The referral process typically begins when primary care providers encounter conditions that exceed their scope of practice, require specialized diagnostic procedures, need interventions not available at the primary level, or fail to respond to appropriate primary care treatment. Good referral systems provide primary care providers with clear guidelines about when referrals are appropriate and which facilities or specialists are most suitable for specific conditions.
Effective referral systems are bidirectional, meaning patients not only move up from primary to secondary to tertiary care when needed, but also step back down when appropriate. A patient who receives cardiac surgery at the tertiary level should transition back to secondary care for specialized follow-up and eventually to primary care for long-term management of their cardiovascular risk factors and other health needs.
Communication between referring and receiving providers is essential for referral systems to function effectively. This includes referral letters that summarize the patient's condition, previous treatments, and specific questions for the specialist, as well as consultation reports that provide recommendations back to the referring provider about ongoing management.
Ayushman Bharat Digital Mission and Health Records
India's Ayushman Bharat Digital Mission represents a comprehensive approach to creating digital health infrastructure that connects patients, providers, and facilities across all levels of care. The mission includes several key components that support integration between care levels and improve continuity of care.
The Ayushman Bharat Health Account provides patients with a digital health identity that can store and share health records across different providers and facilities. This digital identity helps ensure that patient information travels with them as they move between different care levels, reducing duplication of tests and improving coordination between providers.
Healthcare provider registries and facility registries create directories that help patients and referring providers identify appropriate specialists and facilities for different types of care needs. These registries include information about provider credentials, facility capabilities, and available services that support informed referral decisions.
Digital health records systems enable secure sharing of patient information between authorized healthcare providers, supporting clinical decision-making and care coordination. When implemented effectively, these systems can reduce medical errors, prevent duplicate testing, and improve the efficiency of care transitions.
The digital infrastructure also supports population health management by enabling tracking of health outcomes, identification of care gaps, and monitoring of quality indicators across different levels of care. This population-level data can inform system improvements and resource allocation decisions.
Telemedicine and Remote Consultation
Telemedicine technologies help extend specialist expertise to primary care settings and underserved areas, reducing the need for patient travel while supporting clinical decision-making at lower levels of care. India has seen substantial growth in telemedicine utilization, particularly following the COVID-19 pandemic, with millions of teleconsultations conducted through various platforms.
Teleconsultations can support referral decisions by allowing primary care providers to discuss cases with specialists before referring patients, potentially avoiding unnecessary referrals while ensuring appropriate ones are made promptly. Specialists can provide guidance on diagnostic testing, initial treatment approaches, and indications for in-person evaluation.
Follow-up care after hospitalization or specialist visits can often be provided through telemedicine, allowing patients to receive ongoing specialist input while remaining in their home communities. This is particularly valuable for chronic disease management, post-operative care, and monitoring of treatment responses.
Telemedicine also supports medical education by allowing primary care providers and other healthcare workers to participate in continuing education programs, case discussions, and consultation with experts without traveling to urban centers. This educational function helps improve clinical capabilities at all levels of care.
Care Coordination and Continuity
Care coordination involves actively managing patient care activities and communications between healthcare providers to ensure patients receive appropriate and timely care. Effective coordination requires designated responsibility for managing transitions between care levels, standardized protocols for common care transitions, and systems for tracking and following up on referrals and consultant recommendations.
Continuity of care means that patients experience their healthcare as connected and coherent, with providers who understand their medical history, current conditions, and individual circumstances. Continuity can be maintained through consistent relationships with primary care providers who serve as medical homes, through shared health records that travel with patients, and through communication between providers at different care levels.
The primary care medical home concept emphasizes that patients should have an ongoing relationship with a primary care provider or team that coordinates their care across all settings and provides continuous, comprehensive care throughout their lives. This medical home serves as the central hub for care coordination and the patient's main point of contact with the healthcare system.
Back-referral processes ensure that patients return to appropriate levels of care after receiving specialized services. Effective back-referral includes clear communication about ongoing management recommendations, medication changes, follow-up requirements, and warning signs that should prompt return to specialist care.
Financing, Insurance, and Financial Protection
Free Drugs and Diagnostics Initiative
The Free Drugs and Diagnostics Service Initiative aims to reduce out-of-pocket expenditures for essential medicines and diagnostic tests by providing these services without charge at public healthcare facilities. This initiative recognizes that even when consultations are free, costs for medicines and tests can create significant financial barriers that prevent people from completing recommended treatments.
Essential medicines lists specify which drugs should be available free of charge at different levels of facilities, with Sub Health Centres providing a basic list of medicines for common conditions, Primary Health Centres offering expanded formularies, and higher-level facilities providing comprehensive medicine coverage including specialty medications.
Free diagnostic services similarly provide point-of-care and laboratory testing without charge, with service menus expanding at higher facility levels. Sub Health Centres provide basic tests like blood sugar and blood pressure measurement, Primary Health Centres add laboratory tests like complete blood counts and basic chemistry panels, and Community Health Centres and hospitals provide comprehensive diagnostic capabilities including imaging services.
The effectiveness of free drug and diagnostic programs depends on consistent supply chain management, quality assurance for medicines and tests, and clear communication to patients and providers about which services are available without charge. When these programs function well, they can significantly reduce the financial barriers that prevent people from accessing needed healthcare.
PM-JAY Insurance for Secondary and Tertiary Care
Pradhan Mantri Jan Arogya Yojana provides cashless health insurance coverage for hospitalization expenses for eligible families, particularly targeting secondary and tertiary care services that can create financial hardship for households. The program covers approximately 12 crore families with annual coverage amounts designed to provide financial protection against major medical expenses.
PM-JAY coverage includes both medical and surgical treatments provided in empanelled public and private hospitals, with pre-defined package rates for different procedures and conditions. This insurance model helps ensure that families can access needed hospitalization without depleting savings or incurring debt, while also providing hospitals with predictable payment for services.
The empanelment process requires hospitals to meet specific quality standards and agree to provide services at predetermined rates, which helps control costs while maintaining access to care. The cashless payment system reduces administrative burden on families while streamlining hospital billing processes.
Coverage decisions under PM-JAY are made through evidence-based processes that consider clinical effectiveness, cost-effectiveness, and population health impact. The program regularly reviews and updates its coverage policies based on emerging evidence and changing disease patterns.
Out-of-Pocket Expenditure Trends
India has made significant progress in reducing the share of healthcare costs paid directly by households, with out-of-pocket expenditures declining from higher historical levels to more sustainable proportions of total health spending. This reduction reflects the combined impact of expanded public healthcare infrastructure, free drug and diagnostic programs, and insurance coverage expansion.
National Health Accounts data show government health expenditure increasing both in absolute terms and as a share of total health spending, reflecting policy commitments to expand public healthcare access. These trends align with global evidence showing that countries with higher government health spending typically achieve better population health outcomes and greater financial protection.
Despite overall improvement, out-of-pocket spending remains a concern for many households, particularly for services not covered by public programs or insurance, for populations not eligible for existing programs, and in areas where public healthcare infrastructure remains limited. Continued efforts to expand coverage and improve service availability are necessary to achieve universal financial protection.
Regional and socioeconomic variations in out-of-pocket spending highlight the importance of ensuring that healthcare financing improvements reach all populations equitably. Vulnerable populations including tribal communities, rural populations, and low-income urban residents require targeted approaches to achieve financial protection.
Universal Health Coverage Progress
India's progress toward universal health coverage involves expanding both service coverage and financial protection to ensure all people can access needed healthcare without financial hardship. This involves strengthening public healthcare infrastructure, expanding insurance coverage, and addressing social determinants of health that affect healthcare access and utilization.
Service coverage expansion focuses on ensuring essential healthcare services are available to all populations, with particular attention to preventive services, primary care, and emergency care that form the foundation of effective healthcare systems. This includes geographic expansion to underserved areas, service expansion to address changing disease patterns, and quality improvement to ensure services are effective.
Financial protection expansion involves reducing barriers to healthcare access through free services, insurance coverage, and other mechanisms that prevent households from experiencing financial hardship due to healthcare costs. This includes both expanding eligibility for existing programs and developing new financing mechanisms for populations and services not currently covered.
Population coverage expansion ensures that universal health coverage benefits reach all population groups, with particular attention to marginalized and vulnerable populations who may face additional barriers to healthcare access. This requires addressing not only financial barriers but also geographic, cultural, linguistic, and social barriers that can prevent people from accessing care.
Financial Barriers and Solutions
Indian Public Health Standards Framework
The Indian Public Health Standards provide detailed specifications for healthcare facilities at each level of the healthcare system, covering infrastructure requirements, human resource specifications, service delivery standards, and equipment and supply requirements. These standards serve as blueprints for healthcare facility development and benchmarks for performance assessment.
IPHS standards are organized by facility level, with separate volumes covering Sub Health Centres, Primary Health Centres, Community Health Centres, and district hospitals. Each volume specifies both essential standards that facilities must meet to provide safe, effective care, and desirable standards that represent goals for facility enhancement.
Infrastructure standards cover facility layout, space allocation, utility requirements, and environmental conditions necessary for safe healthcare delivery. These standards ensure that facilities have appropriate space for patient care, privacy for consultations, and infection prevention capabilities.
Service delivery standards specify which healthcare services should be available at each facility level, including clinical services, diagnostic capabilities, and support services. These standards help ensure appropriate distribution of healthcare capabilities while avoiding duplication of expensive services.
Equipment and supply standards detail the medical equipment, instruments, medicines, and other supplies necessary for facilities to deliver their specified services effectively. These standards support procurement planning and help ensure facilities have necessary resources for quality care delivery.
Workforce Planning and Skill Development
Healthcare workforce development involves planning for current and future healthcare human resource needs, developing educational programs that prepare workers with necessary competencies, and creating career development pathways that retain skilled workers in the healthcare system.
Medical education expansion has increased the number of medical colleges and MBBS seats substantially over the past decade, addressing long-standing shortages in physician availability. Similarly, nursing education expansion has increased capacity for training nurses and other healthcare workers needed across all levels of care.
Skill development programs provide training for existing healthcare workers to expand their competencies and adapt to changing healthcare needs. Community Health Officer training programs, for example, prepare healthcare workers to provide expanded primary care services at Health and Wellness Centres.
Continuing education and professional development ensure that healthcare workers maintain and update their skills throughout their careers. This includes both formal continuing medical education requirements and informal learning opportunities through mentoring, case discussions, and quality improvement activities.
Workforce distribution remains a challenge, with rural and underserved areas often facing shortages of healthcare workers despite overall increases in healthcare workforce supply. Addressing this challenge requires both incentive programs to encourage service in underserved areas and career development opportunities that make rural service attractive to healthcare professionals.
Quality Improvement and Patient Safety
Quality improvement involves systematic efforts to enhance healthcare processes and outcomes through measurement, analysis, and implementation of improvements. Patient safety focuses specifically on preventing harm to patients through healthcare processes and creating systems that minimize risks and respond effectively when adverse events occur.
Quality measurement involves tracking indicators of healthcare process and outcomes to identify opportunities for improvement and monitor progress over time. This includes clinical quality measures like infection rates, treatment outcomes, and patient safety indicators, as well as patient experience measures and system performance indicators.
Quality improvement methodologies provide structured approaches for identifying problems, developing solutions, implementing changes, and monitoring results. These methodologies can be applied at individual facility levels and across healthcare systems to drive systematic improvements.
Patient safety systems include processes for identifying and reporting adverse events, analyzing root causes of safety problems, implementing preventive measures, and creating cultures that prioritize safety over blame. Effective patient safety systems learn from errors and near-misses to prevent similar problems in the future.
Accreditation and certification programs provide external validation of healthcare quality and safety standards, creating incentives for continuous improvement while providing assurance to patients and payers that facilities meet established standards.
Key Takeaways
Public health systems organize care into primary, secondary, and tertiary levels because this structure delivers better population health outcomes more efficiently than unorganized approaches. Primary care serves as the accessible foundation that handles most health needs through prevention, early intervention, and management of common conditions. When primary care is strong and accessible, it prevents many conditions from progressing to stages requiring expensive interventions at higher levels.
Secondary care provides specialized services that bridge between community-based primary care and hospital-based tertiary care, handling conditions that exceed primary care capabilities while referring the most complex cases to tertiary facilities. Tertiary care delivers advanced treatments while driving innovation through research and education, but its resource intensity requires careful coordination with lower levels to ensure appropriate utilization.
The effectiveness of this system depends entirely on integration between levels through referral systems, information sharing, and care coordination. Digital health technologies are enhancing these connections by enabling remote consultations, shared health records, and better communication between providers. Financial protection through free services and insurance coverage reduces barriers to accessing appropriate care at each level.
For patients and families, understanding this system helps you start at the right level for your healthcare needs, advocate effectively for appropriate referrals when needed, and take advantage of free services and financial protection available through public programs. For students and healthcare professionals, this framework provides essential context for clinical decision-making, care coordination, and system improvement efforts.
Looking ahead, success in strengthening healthcare systems will require continued investment in primary care infrastructure, workforce development, technology integration, and quality improvement across all levels of care. The goal is creating healthcare systems that work for everyone - accessible, affordable, effective, and continuously improving to meet evolving population health needs.
Whether you are navigating healthcare for yourself or your family, preparing for healthcare career examinations, or working to improve healthcare delivery in your community, understanding how these three levels work together provides the foundation for more informed decisions and more effective advocacy for better healthcare for all.
